AMPLIFY VOL. 38, NO. 1

The healthcare sector stands at a crossroads, confronted with the dual challenge of dealing with the health impacts of climate change while reducing its own substantial carbon footprint. With global emissions from the sector projected to triple by 2050, there is a dire need for immediate, decisive action. Healthcare organizations must integrate sustainability into their operations to ensure their long-term viability and improved health outcomes.
The healthcare sector accounts for 10% of the world’s GDP, or US $7.2 trillion annually; it also contributes to 4.4% of global net emissions.1 To put this into context, if the healthcare sector was a country, it would be the fifth-largest emitter of greenhouse gases (GHGs) in the world.
Unless action is taken, the sector’s global emissions will reach 6 gigatons a year by 2050.2 Factors such as air pollution, water pollution, and climate change contribute to the burden of disease, not least in the form of cardiovascular disease and cancers, creating pressure on health systems. How can the healthcare sector resolve the paradox of being responsible for both the cause and the care?
Many healthcare organizations are implementing environmentally friendly practices to reduce their carbon footprint, make more sustainable use of their resources, and deliver results on the triple bottom line of people, profits, and the planet. They do this knowing that sustainability intersects with other priorities such as a rising demand for health services, spiraling healthcare costs, quality of health outcomes, and patient satisfaction. For sector participants and their stakeholders, adopting environment-friendly practices is not just a moral obligation, it is also a strategic necessity with sizeable financial, reputational, and population-health implications.
Regulatory pressures are also increasing, with stricter reporting requirements and penalties for noncompliance creating urgency. Healthcare organizations that proactively commit to sustainability stand to benefit not only from cost reduction but also by building trust and credibility with patients, regulators, and investors. Embedding sustainability offers a path to environmental responsibility, financial performance, and operational excellence.
In this article, we introduce a framework for improving the healthcare sector’s environmental performance based on three steps: green practices, green initiatives, and green environment enabled by digital solutions.
Green practices focus on energy efficiency, optimizing waste management, and adopting circular economy practices to tackle the sector’s environmental inefficiencies. Green initiatives drive clinical and operational changes such as new models of care, service-line management, clinical pathway redesign, and digital/AI adoption. Finally, green environment addresses cultural and stakeholder-related barriers in the wider health system to enable long-term environmental and operational resilience.
The Hidden Cost of Healthcare
Healthcare facilities are the cornerstone of most health systems and where the sector’s environmental impact can most easily be observed. Hospitals operate 24/7 and typically consume between 2,000 and 4,000 kWh per bed annually on energy for lighting, heating, ventilation, and medical equipment (equivalent to 3,000-10,000 kg of carbon dioxide equivalent [CO2e] in emissions).
The healthcare sector also generates substantial waste, including single-use and disposable materials, which can amount to almost 2,000 kg of CO2e per bed per year from medical and general waste. Operating rooms occupy a relatively small physical area in a hospital but produce 20%-33% of a facility’s total waste. It is estimated that 15% of hospital waste is hazardous and can be infectious, toxic, or radioactive, with hospitals in high-income countries producing up to 11 kg of hazardous waste per bed per day, much of which is not biodegradable.3,4
Orthopedics, oncology, cardiology, and neurology departments have the highest carbon footprint because of their extensive use of energy-intensive equipment (e.g., operating rooms, intensive care units, and imaging machines), single-use materials, and gases. In nephrology, dialysis contributes significantly due to high water and energy consumption. In hospitals, support functions such as facilities management, IT, and catering stand out as chief contributors.
The scale of the problem is also challenging beyond the four walls of a hospital, with the healthcare supply chain responsible for more than 70% of the sector’s emissions, primarily from fossil fuel consumption in the production, transport, and disposal of drugs, devices, and supplies.
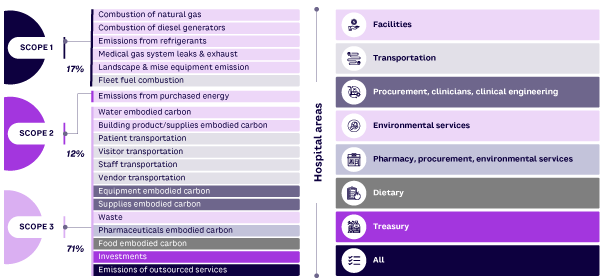
The manifestation of emissions at a hospital level is shown in Figure 1,5 split across Scope 1 (direct), Scope 2 (indirect via energy usage), and Scope 3 (all other indirect sources, including supply chain). This highlights the need for a comprehensive approach that extends beyond hospital operations.
Solutions for Healing Healthcare
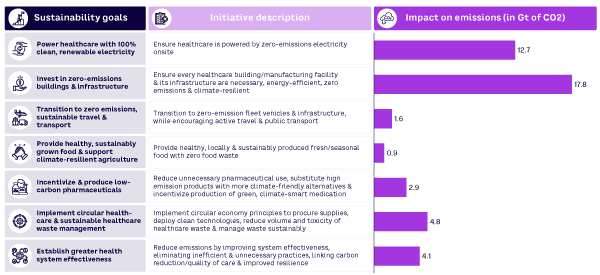
The healthcare sector can embrace sustainability without compromising quality of care or impairing patient experience (see Figure 2).6 Advances in green technologies such as alternative energy sources, water conservation systems, and waste-reduction measures, particularly in sterile zones such as operating rooms, offer significant potential for reducing environmental impact.
International energy regulations and standards provide complementary guidelines that can be integrated into broader sustainability efforts. Infrastructure and real estate standards such as LEED (Leadership in Energy and Environmental Design) inform energy-efficient building design; ASTM (American Society for Testing and Materials) provides standards for environmental site assessments; and BREEAM (Building Research Establishment Environmental Assessment Method) certifies the sustainability performance of buildings. From a management perspective, International Organization for Standardization (ISO) 14001 provides a framework for organizations to improve their environmental performance, and the US program Energy Star certifies energy efficiency.
The Global Green and Healthy Hospitals (GGHH) network and the International Hospital Federation (IHF) also provide resources to help hospitals reduce their environmental footprint as part of a knowledge-sharing community. These standards yield substantial cost savings, enhance operational efficiencies, and encourage cross-industry collaboration and partnerships that can drive systemic change and innovation in sustainable healthcare practices.
We can also look to leading healthcare organizations that have successfully integrated sustainable practices into their operations:
-
The University Medical Center of Princeton (New Jersey, USA) reduced energy use by 30% with sustainable design features like a green roof and energy-efficient lighting.
-
Cleveland Clinic (Ohio, USA) installed LED lights and solar arrays, reducing its energy use and GHGs by 30%. By replacing disposable items with reusable or compostable alternatives, the Mount Sinai Health System (New York, USA) reduced its use of single-use plastics and cut waste by 15% in the first year.
-
The Lucile Packard Children’s Hospital Stanford in California, USA, implemented a comprehensive water management plan that reduced its water usage by 38%.
-
National Health Service (NHS) England, which is responsible for more than 500 hospitals, is targeting net zero emissions by 2040 for Scope 1 and 2 and by 2045 for Scope 3. Strategies such as reusing medical instruments have saved more than £250,000 annually for some hospitals.
At a national level, the UK’s NHS Sustainability Action Plan and the US’s Sustainability Action Plan aim to reduce the sector’s carbon footprint and enhance sustainability. Both plans include a variety of initiatives, from energy efficiency and transportation to sustainable procurement and partnerships. Each plan addresses unique regional challenges, but they share the overarching goal of achieving net zero emissions and promoting environmentally responsible healthcare practices.
NHS Sustainability Action Plan (UK)
-
Developing frameworks to assess carbon reductions in new care models
-
Transitioning to zero-emission vehicles, including the world’s first zero-emission ambulance
-
Planning to construct 40 net zero hospitals, adhering to carbon-neutral standard
-
Utilizing $60 million LED lighting replacement program to enhance patient comfort & save energy
-
Collaborating with suppliers to align the medicine supply chain with net zero emissions targets by the end of the decade
Sustainability Action Plan (US)
-
Targeting 100% carbon pollution-free electricity through renewable energy
-
Transitioning to zero-emission vehicle fleets
-
Achieving net zero emissions in buildings by enhancing energy & water efficiency
-
Expanding recycling & minimizing construction debris
-
Updating sustainable procurement practices & conducting staff training in climate literacy through outreach programs
-
Addressing climate impacts on underserved communities
-
Accelerating sustainability & climate initiatives through partnerships with federal agencies & private organizations
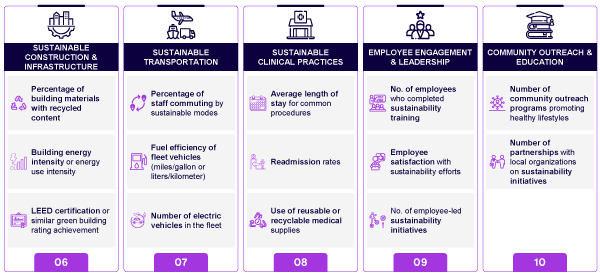
Global healthcare entities are adopting a range of KPIs to monitor and measure the effectiveness of their sustainability efforts (see Figure 3). These measurements help track progress and ensure alignment with global environmental goals, such as COP28 and the Paris Agreement, as well as national CO2e targets.

The Road to Environmental Performance
In Arthur D. Little’s (ADL’s) work with healthcare clients, we encourage a three-step approach to improving environmental performance (see Figure 4). By addressing environmental, economic, and operational practices at all levels, from core principles to societal integration, healthcare organizations can systematically work toward their sustainability goals and realize long-term benefits at a facility, system, and population level.
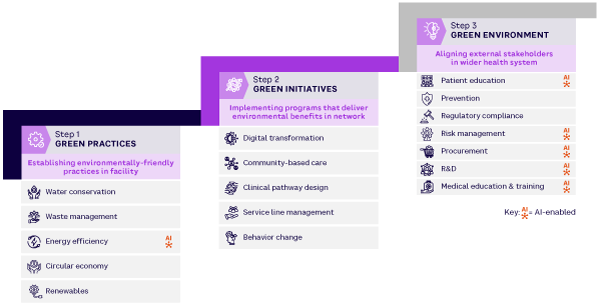
Green Practices
As a first step, organizations should focus on fundamentals such as water conservation, waste management, energy efficiency, circular economy principles, and investment in renewable sources (e.g., wind turbines, solar panels, and biomass energy). For example, waste-to-energy systems that convert medical waste into usable energy offer a dual benefit of waste reduction and energy generation and have been successfully implemented by several European hospitals.
These basic activities reduce the environmental footprint of healthcare operations and lay the foundation for sustainable progress, starting with Scope 1 and Scope 2 emissions.
Green Initiatives
The next step is to integrate sustainability into broader operational areas, recognizing the impact of initiatives like community-based care, clinical pathway redesign, behavioral change, and service-line management can have on Scope 1 and Scope 2.
Telemedicine is being adopted at a good pace, in part because of a ramp-up during the recent pandemic. Virtual consultations reduce the need for physical visits, decreasing carbon emissions associated with transportation while lowering the demand for physical infrastructure such as clinic space. Diagnostic tools can reduce the frequency of unnecessary tests and procedures, lowering resource consumption and patient visits. More robust demand prediction can minimize waste from unused, short-shelf-life drugs and supplies.
Redesigning the model of care to focus on well-being and healthy living, as well as care in alternative settings, can reduce resource consumption and hospital visits while enhancing patient experience and convenience. Linked to this, standardized clinical pathways streamline care processes and reduce unnecessary interventions, leading to more efficient resource use and minimized waste. Hospitals can optimize staffing, scheduling, and patient flow and reduce the need for some patient tests and travel, lowering the environmental impact of healthcare.
Green Environment
The third step is to tackle complex challenges that require stakeholder alignment, such as patient education, procurement, regulatory compliance, and risk management. This step also focuses on long-term enablers such as prevention, medical education, and R&D to ensure sustainability becomes deeply integrated into healthcare delivery.
Wearable devices can monitor patient health in real time, alerting the patient/caregiver/provider about potential health issues before they escalate. The Scope 3 implications of such technologies, however, need to be weighed against the potential benefits. In post-discharge scenarios, they can prevent avoidable readmissions and thus lower the resources consumed by emergency visits and rehospitalization.
With Scope 3 emissions accounting for around 70% of the sector’s GHGs, procurement is key to greening the healthcare supply chain. Procurement teams must collaborate with suppliers to improve transparency and reduce emissions. For example, they can consider the potential reusability of medical instruments, reduced need for packaging, and recyclability of the materials used to manufacture their products. Balancing sustainability with cost, quality, and performance requires thoughtful compromises. Healthcare organizations can adopt eco-friendly procurement strategies, focusing on reducing single-use plastics, sourcing sustainably, and ensuring supplier adherence to environmental standards
R&D can leverage AI to minimize resource consumption and environmental waste in clinical trials and drug discovery (e.g., modeling the impact on certain patient segments without sourcing new datasets). This can lead to a more streamlined process that balances innovation with sustainability goals.
Increasing physician awareness of healthcare’s environmental impact and integrating best practices into medical education and training is essential for promoting sustainability. AI tools, such as those used to diagnose diabetic retinopathy, can help clinicians make more accurate diagnoses and choose optimal treatments, resulting in faster recoveries and reducing the need for more complex procedures, ultimately leading to lower resource consumption.
Overcoming Challenges
The high up-front costs of implementing green technologies, the complexity of regulatory requirements, and difficulties capturing and reporting data pose significant hurdles. The fragmented nature of the healthcare industry, with its mix of public and private providers, further complicates efforts.
One of the major barriers to sustainable transformation is the significant financial investment required to upgrade existing (often aged) facilities with energy-efficient systems. Renewable energy systems, energy-efficient HVAC systems, and sustainable building materials often require substantial up-front costs that can take years to recoup. Lenders and investors are increasingly factoring in environmental, social, and governance (ESG) criteria when assessing credit risk and financing terms, as these considerations can greatly influence an organization’s long-term financial performance and sustainability.
Decisions about investing in care versus investing in the environment, and issues around short-term capital-funding constraints, can be simplified through public-private partnerships (PPPs) and private-sector participation (PSP) contracts designed to fund large-scale capital projects and provide access to best-practice solutions.
Healthcare organizations must navigate a complex regulatory environment, often involving multiple agencies that have their own stringent standards. Any changes to operations, such as adopting a new waste management system, must comply with these regulations, which can hinder implementation. Taking proactive steps toward integrating sustainability into their operations, reporting, and ensuring compliance with standards will ensure healthcare organizations are better positioned to meet these requirements and avoid potential fines or penalties.
A commitment to decarbonization requires setting clear, achievable carbon-reduction targets and developing a plan to implement and monitor results. This entails gathering detailed activity data (bottom-up) from internal sources relating to transportation, energy consumption, waste production, and material usage. This is challenging enough for most organizations. Getting accurate and reliable data from suppliers on Scope 3 emissions is even harder due to data availability, data quality, and restrictions on data sharing. A collaborative approach that balances rewards and incentives and accommodates trade-offs in product cost, quality, and performance is needed.
A Sector-Wide Responsibility
Effective decarbonization in healthcare requires coordinated efforts from various stakeholders, each playing a critical role in driving sustainability, as we explore below.
Regulators
-
Establish standards that encourage existing facilities to modernize and upgrade. Issue regulations to guide new facility development.
-
Introduce regulations for healthcare facilities to report their emissions targets and performance. Regulations should include clear, measurable goals and timelines, with regular audits and penalties for noncompliance.
-
Support R&D in energy-efficient technologies and renewable energy sources.
-
Facilitate partnerships and PPP/PSP contracts; provide incentives like sustainability credits, grants, or tax breaks for hospitals meeting emissions standards.
Healthcare providers
-
Identify and implement KPIs to track progress in carbon-emissions reduction with regular monitoring to ensure continuous improvement and data-driven decisions.
-
Report sustainability performance to regulatory bodies to demonstrate commitment and ensure compliance with industry standards. Hospitals should prepare annual sustainability reports detailing their energy use, carbon emissions, and overall environmental performance.
-
Build a culture of sustainability to empower staff to actively participate in decarbonization efforts. Hospitals should educate staff on best practices and raise awareness through internal campaigns.
Payers
-
Design pricing models that reward hospitals for implementing sustainable practices. Premiums can be reduced for hospitals that meet targets to encourage widespread adoption of carbon-reduction efforts.
-
Support initiatives like sustainability credits or lower premiums for hospitals meeting emission standards. This can create a competitive advantage for green hospitals.
-
Partner on projects or fund sustainable upgrades to reduce overall healthcare costs. Payers should work with hospitals to develop joint initiatives that align sustainability objectives with premium healthcare standards.
Suppliers
-
Provide sustainable products that are manufactured using low-carbon processes and sustainable materials and that minimize packaging waste.
-
Ensure transparency in supply chain emissions by providing data on the carbon impact of products. Healthcare organizations should be able to make informed purchase choices according to information on how materials were sourced, produced, and delivered.
-
Partner with hospitals on joint sustainability projects to develop eco-friendly products and packaging, reduce transportation emissions, and lower disposal costs.
Conclusion
Sustainability in healthcare is a strategic imperative that can drive cost savings, enhance patient care, and improve an organization’s reputation with stakeholders. By investing in green technologies, optimizing supply chains, and adopting sustainable practices, healthcare organizations can contribute to a healthier planet and ensure their long-term success in an increasingly competitive and environmentally conscious world.
References
1 Karliner, Josh, et al. “Health Care’s Climate Footprint.” Healthcare Without Harm/Arup, Green Paper No. 1, September 2019.
2 “Global Road Map for Health Care Decarbonization.” Healthcare Without Harm/Arup, Green Paper No. 2, September 2021.
3 Tieszen, M.E., and J.C. Gruenberg. “A Quantitative, Qualitative, and Critical Assessment of Surgical Waste. Surgeons Venture Through the Trash Can.” JAMA, Vol. 267, No. 20, May 1992.
4 Janik-Karpinska, Edyta, et al. “Healthcare Waste — A Serious Problem for Global Health.” Healthcare, Vol. 11, No. 2, January 2023.
5 Karliner et al. (see 1).
6 Health Care Without Harm/Arup (see 2).




