AMPLIFY VOL. 37, NO. 6

The healthcare and pharmaceutical industries are witnessing a surge in digital data generation thanks to wearable sensors, electronic health records, and clinical and genetic data.1 Simultaneously, the emergence of data-centric decision-making is set to benefit healthcare services in several areas.
These areas include:
-
Genomics and precision medicine. This will enable targeted treatments for specific patient groups, potentially enhancing efficacy and leading to novel therapeutic avenues.
-
Remote care. This will enhance healthcare accessibility, leading to patient needs being addressed earlier and the healthcare system potentially becoming more efficient.
-
Technology-supported self-management. Patients will be able to better understand their condition(s), helping them more effectively manage their health and fostering improved behavioral and clinical outcomes.
-
Data. This will serve as a catalyst for improving national healthcare systems’ research and decision-making.
-
AI. This could augment analytical capabilities for patient diagnoses, leading to more efficient triage and patient logistics management.2
The continued development of healthcare-related technologies, including AI, is transforming healthcare business processes, especially in medium-sized and large pharmaceutical firms, resulting in faster, more efficient decision-making. Other advantages include diminished human error and accelerated product development cycles, ultimately resulting in faster product launches.
Meaningful Metrics
In recent years (and in large part because of the pandemic), governments stepped up pressure on the healthcare and pharmaceutical sectors, asking them to develop a more aligned, cohesive approach to the use of digital technologies and data management in decision-making to deliver greater value to stakeholders.3
Aligning healthcare interventions with outcomes that matter to patients is of paramount importance. Significant challenges arise when healthcare systems prioritize activity and inputs over outcomes, hindering adoption. For example, researchers found payer uncertainty about the value of investment in mental health treatments and showed the potential for this to impede the adoption of new treatments.4
Two other research groups demonstrated the criticality of aligning on outcome metrics to achieve value-based healthcare (VBHC).5,6 Meaningful metrics and measurements serve as a guiding condition for innovation implementation, informed decision-making, quality improvement, and reduced costs.
A recent initiative spearheaded by the Welsh Government demonstrates the critical role of robust digital infrastructure in driving innovation adoption and realizing tangible outcomes. The Ibex Galen AI platform’s analysis of prostate biopsies resulted in a remarkable 13% increase in cancer detection, and the platform is now being used at Betsi Cadwaladr University Health Board to examine suspected breast cancer cases.
Funded through the Welsh Government’s innovation fund and supported by the Small Business Research Initiative (SBRI) Centre of Excellence, the AI tool uses a traffic-light system to classify digital images of pathology samples to indicate the likelihood of cancer, helping clinicians prioritize urgent cases. This is leading to faster diagnoses and is expected to reduce the need for additional biopsies and tests.7
Research Methodology
This article is informed by in-depth discussions with 48 leaders in senior management positions in healthcare and pharmaceutical organizations. The primary data was collected through a series of interviews, each lasting 45 to 60 minutes.
Each interview consisted of a series of questions related to collaboration activities between healthcare and pharmaceutical organizations and their use of technology platforms to deliver value to stakeholders. The questions sought to elucidate the best practices and challenges surrounding the collaborative use of emerging technology and data-centric decision-making to deliver value to stakeholders.
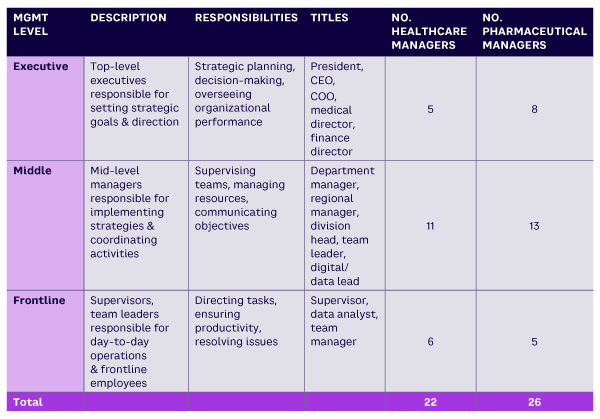
The interviews were recorded and transcribed in preparation for thematic analysis. Most participants held mid-level executive positions in their organization (n=37), with roles varying from managing director to division head and data lead. The remaining candidates (n=11) held roles such as supervisor, data analyst, and team manager (see Table 1).
Key Barriers
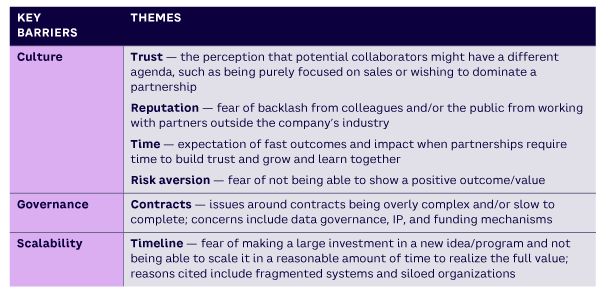
A qualitative data analysis was performed to surface themes related to developing an environment conducive to embedding technology platforms and data analytics for collaborative value provision (see Table 2).
The key barriers were each considered from a practitioner viewpoint to reveal themes (and contexts) and establish best practices (see Figure 1).
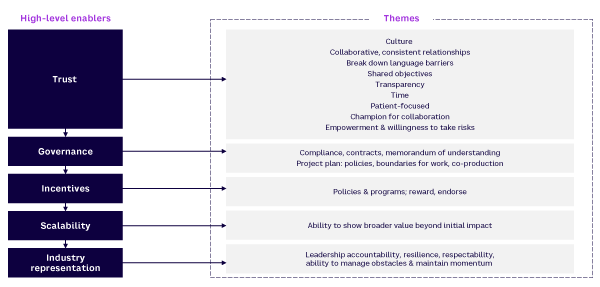
Trust
Many participants viewed trust as critical for collaborations to flourish and noted that partners must take a consistent approach to developing strong relationships:
-
Establish a common language.
-
Understand the healthcare system.
-
Align with others to create a shared agenda.
-
Set clear shared objectives, including joint accountability.
-
Name a champion for the collaboration.
-
Establish alignment at all levels of an organization (leaders, managers, and subject-matter experts).
-
Ensure experienced clinical champions are empowered and willing to take risks.
Governance
Respondents said a memorandum of understanding is the best way to achieve strong, enabling processes. These documents should be co-created with legal experts from the outset and should include a requirement for a clear project plan, enabling SOPs (standard operating procedures), and ownership and financial boundaries.
Participants frequently expressed frustration with the intricate nature of contractual agreements, which can hinder the swift progression of collaborative initiatives. Delays in finalizing contracts not only impede project timelines, they exacerbate uncertainties surrounding data ownership, rights to innovations, and financial arrangements. Addressing these concerns requires a streamlined approach to contract negotiation and execution, one that favors clarity and expediency in addressing crucial aspects, such as data management, intellectual property (IP) rights, and financial obligations.
Incentives
Performance management systems explore the interplay between monetary and nonmonetary incentives, resulting in policies or programs that reward the right collaborations and endorse and motivate individuals and teams. Susanna Gallani, the Tai Family Associate Professor of Business Administration at Harvard Business School, has examined mechanisms to align behavior, reward performance, and reduce burnout. A major part of her current work focuses on innovations in incentive models in healthcare.8
Scalability
In this case, scalability means the ability to demonstrate from the outset how learnings might have value implications beyond initial impacts. For example, concerns around timelines stem from a fear of investing in new ideas/programs without the ability to scale them within a reasonable time frame due to fragmented systems and organizational silos.
Industry Representation
As expected, the collaboration of healthcare systems with pharmaceutical companies is a key requirement in the successful integration of new data technology platforms. The pharmaceutical or technology companies’ effort should be headed up by a senior executive who understands the system, is highly motivated, is willing to be held accountable for revenue generated (or not), is bold, and can manage the challenges associated with maintaining momentum.
Recommendations
With best practices/enablers established, the next step is to use the right individuals to choose effective tools and establish robust processes, as described below.
Right Tools
Highly interoperative technology that allows safe data capture and robust data management is critical to ensuring data can flow from patients to clinicians and then across the total pathway of care.
Right Processes
When healthcare entities form partnerships, whether it’s with pharmaceutical companies to explore new drugs/treatments or with IT companies to implement new data technologies, the contracting arrangements tend to be protracted due to their complexity.
Developing a consistent approach that is both robust and nimble requires careful co-development. The governance framework must account for resource and financial flexibility as well as:
-
Metrics and measurements. The underlying principle of VBHC is delivering outcomes that matter to patients at the same or lower cost. Of course, understanding and evaluating existing or new interventions requires robust metrics that are focused on patient outcomes, rather than activity or outputs. It’s also important to implement incentives, policies, or programs that reward the right collaborations and endorse and motivate individuals and teams to work together. These must be carefully designed to ensure the focus remains on value and doesn’t get replaced by activity volume.
-
Pathway mapping. Creating and evaluating interventions begins with understanding the entire cycle of care, not just the point in the pathway where a new intervention may have an impact. For individual patients, having choices at various points in the care pathway enhances their sense of empowerment and involvement in their treatment. This holistic perspective helps design interventions that are more effective and better integrated into the patient’s complete healthcare experience. In the health research sector, an understanding of the total care cycle leads to greater confidence in partnering with health systems and enables broader consideration of innovative services that create value (e.g., diagnostics, remote monitoring, and community services).
Right People
Many survey participants emphasized that in addition to a strong, knowledgeable leader, successful collaborations need a supportive environment. Many respondents expressed concern over the risk of relying on a single individual, potentially jeopardizing programs. It is crucial to have organizational alignment and support from skilled leaders who can manage new and complex partnerships. Additionally, having the right resources and skills from other team members readily available and deployed is essential. Here are four key elements:
-
Culture. The culture must actively support collaboration, including leaders with a flexible mindset, an ability to embrace diversity of thought, and an understanding that successful strategic partnerships require time to develop. Every organization and industry has its own jargon, to the point where it’s almost a language. Thus, each partner must spend time learning the “language” of the other collaborators.
-
Functions. Success is predicated on having a cross-functional team that includes individuals with clinical, financial, legal, and management expertise.
-
Team. The importance of diversity of thinking and skills was explicit in the interviews, from negotiating a collaboration and securing endorsement from the right leaders across the respective organizations to designing the program. The latter involves having the right clinical experts from the entire pathway, the right analysts to support evaluation, the right technology experts, the right compliance experts, and the right communications experts. This requires strong project management skills to ensure subject matter experts are engaged and included while avoiding management by committee, over-consultation, and/or program paralysis.
-
Industry representation. Strong leadership from pharmaceutical and/or technology companies is critical to the success of a collaboration. Our survey identified the following competencies as critical:
-
Strategic vision — understands the healthcare landscape and aligns business vision and portfolios to create compelling proposals; turns ideas into actions; and has a proven track record of delivering successful outcomes
-
Resilience and agility — can shift priorities in response to the needs of customers or the organization; has an openness to learn from mistakes and take well-reasoned risks; finds solutions and makes decisions despite incomplete information; inspires others to engage through collaboration; demonstrates optimism; and guides programs forward in challenging circumstances
-
Analytical thinking — can identify areas of shared interest; can analyze appropriate data to formulate approaches; explores various options to deliver value for all collaborators; and sets out a clear process for reviewing outcomes
-
Courageous leadership — a driven, courageous leader who can manage obstacles and challenges while maintaining focus on the program’s critical path; has the confidence to make decisions at a local level on behalf of the organization and, where necessary, to slow or accelerate activity
-
Emotional intelligence — creates a compelling vision; supports and builds strong internal and external stakeholder relationships; demonstrates an ability to engage other functions; and presents with confidence and gravitas
-
Conclusion
The healthcare and life science sectors are under increasing social and economic pressures locally, nationally, and globally. Merely increasing spending on healthcare is not resolving these issues. Harnessing new technologies and enabling data-centric decision-making will be pivotal for transforming how we deliver healthcare, and collaboration with pharmaceutical and technology companies will be essential to improving patient outcomes. We hope our findings will contribute to an evolving blueprint that leads to greater success in collaborative partnerships and transformational initiatives for patient, societal, and economic benefits.
References
1 Johnston, William, et al. “Reliability, Validity and Utility of Inertial Sensor Systems for Postural Control Assessment in Sport Science and Medicine Applications: A Systematic Review.” Sports Medicine, Vol. 49, No. 5, May 2019.
2 Castle-Clarke, Sophie. “What Will New Technology Mean for the NHS and Its Patients? Four Big Technological Trends.” The Health Foundation/Institute for Fiscal Studies/The King’s Fund/Nuffield Trust, 2018.
3 “Digital and Data Strategy for Health and Social Care in Wales.” Welsh Government, 27 July 2023.
4 Wang, Philip S., Christine M. Ulbricht, and Michael Schoenbaum. “Improving Mental Health Treatments Through Comparative Effectiveness Research.” Health Affairs, Vol. 28, No. 3, May/June 2009.
5 “Value Based Healthcare: Learning from Practice.” King’s Health Partners, accessed June 2024.
6 Gabriel, Lucinda, et al. “Value-Based Healthcare Analysis of Joint Replacement Surgery for Primary Hip Osteoarthritis.” BMJ Open Quality, Vol. 8, No. 2, June 2019.
7 “AI Helping to Diagnose Cancer in Wales.” Welsh Government, 27 July 2023.
8 Gallani, Susanna. “Conduit Incentives: Eliciting Cooperation from Workers Outside of Managers’ Control.” Accounting Review, Vol. 93, No. 3, 2023.






